Prior Authorization
8 Vendor Reviews
This 2023 review of prior authorization tools and services inspects the background issues driving the rising PA syndrome and the associated labor costs to physicians using the latest data from the American Medical Association, the AAFP, and the Counsel for Affordable Quality Healthcare CAQH. Compare steps to action, review solutions and discover a checklist with names and reviews of the top 8 vendors that supply today’s best prior authorization solutions.
What is Prior Authorization?
The American Medical Association defines prior authorization as any process by which physicians and other health care providers must qualify for payment coverage by obtaining advance approval from a health plan before a specific service is delivered to the patient. It goes on to say, “As a health plan cost-control process it is overused, costly, inefficient, opaque and responsible for patient care delays.”
Prior Approval is an aspect of utilization management, specifically prospective utilization review, where an insurance payer looks at a number of factors such as medical necessity, prior treatment, clinical indications, and total therapy cost to determine whether a cost-savings can occur.
Synonyms: PA is also commonly referred to as precertification, prior notification, prior approval, prospective review, prior review; and the colloquial pre-cert, pre-auth and prior-auth commonly used by specialist; as is the conversational shortened-form: “auth”. Example: Have you obtained the auth for that patient yet.
Utilization management is practiced by both insurance payers and hospitals to rein in costs and reduce denials, but today, PA is responsible for 92% of care delays, treatment abandonment, and 853 hours per year of wasted staff time. Action must be taken. This 2023 review is about regaining control at the physician’s practice by implementing electronic prior authorization (ePA) as your primary method of obtaining prior approval.
Prior Authorization Calculator
Calculate the Impact Prior-Auth is Having on Your Practice

Six Things You Need to Know Now
- Doctors have to change, as obtaining preauthorization manually over fax and phone has become unsustainable, and going electronic is inevitable. States are now beginning to mandate that payers adopt EDI standards for benefit determinations. And payers themselves are already on the move as the last 18 months have witnessed a 38% rise in PA requirement. This trend will only continue until the majority of prior approvals are processed electronically similar to e-prescribing and electronic claims.
- Changing now can mean a sharp decrease in wasted time and money – as much as a factor of 5 times – translating to less labor (meant less expense) for you and your staff, and time freed up to see more patients.
- Presently, just 70 payers accept the ANSI 278 electronic service authorization form, but they are the seventy largest, and represent over 80% of all eligibility, claims and authorizations.
- You will still need some manual processing, but in some cases (as with PracticeSuite), it can be outsourced to the vendor who is helping you with electronic preauthorization (ePA).
- Expect to pay in the neighborhood of $7 for each electronic PA. The industry average labor cost of processing a complex PA manually is $35 – $100.
- You have a choice of ePA vendors, but the best solutions are ones that integrate seamlessly within your EHR and practice management system through API’s, or an HL7 interface.
Background
On average physicians obtain 29 medical approvals per week, while 23 percent of physicians report they and their staff complete more than 40 PA requests per week. Eighty percent of physicians report they are either sometimes, often or always required to repeat PA requests for prescriptions when the patient has already been stabilized on a treatment. And 86% of physicians report PA burdens have increased over the past five years, while the AMA projects to expect an increase of 20% per year in PA requirement.
Finally, 80% of requests for prior approval cannot be completed without responding to clinical questions or submitting clinical records. The AMA reports that precertification consumes approximately 1 hour of physician time, 13.1 hours of nurse time, and 6.3 hours of clerical time per week – or 853 hours per year of staff time, costing $82,975 in labor annually per full time physician.
Time Is Money
According to a study published on HealthAffairs, when that time is calculated in dollars, median spending for a primary care practice to obtain PA is $47,707 per full time physician––or $23 billion and $31 billion annually industry wide.
According to the most recent study conducted by McKesson using data from CAQH––the organization that monitors electronic adoption in healthcare; when faxes, phone calls, clinical time and other aspects are considered, labor costs to a doctor range from $35 to $100 per prior approval.
In 2016, 82% of pre-authorizations were done manually over the phone and fax, but during 2017, electronic adoption dropped from a high of 18% to just 8% today. During this same time period, pre-authorization cost rose $1.8 billion, while the rate of administrative transactions to process them increased 38%.
According to CAQH, health care providers could save $7.5 billion annually by switching on electronic authorizations, but other groups like the AMA put the potential savings to physicians at two to three times that.
Do you know just how much precertifications are costing you each month? Calculate the impact and, the saving you could experience by switching to electronic PA.
Authorization Desk
The Problem
Providers and their staff report obtaining PA as time consuming, expensive, and frustrating. The AMA reports 84% of doctors surveyed reported that their preauthorization burden was high or extremely high.
Limited Commonality
Given the complexity, limited commonality, and frequency of changes among both payers and plans, out of 1,300 procedure-specific authorization policies among 23 major health plans, only aneight percent commonality exist between plans (e.g. patient demographics). Then there are sub-plans that can require a separate PA from a third party.
Not having a required PA in place ultimately results in a denied reimbursement, and due to direct loss of revenue from denial of payment by insurances––referred to as fatal denials, official estimates place PA cost to the provider at $82,000 per year. And a recent study by MGMA shows that PA is on the rise.
Impact on Doctors
After EHR, PA is the number two cause of job dissatisfaction among physicians. And of the hundreds of hours that doctors spend interacting with insurances each year to process PA, none of it is reimbursed by insurance companies, representing an egregious and injurious burden placed upon providers who are bound by oath, by desire, and by law to provide the best possible healthcare for their patients. Resources spent on bureaucracy are resources that are ultimately unavailable to patients.
Impact on Patients
Patients suffer directly when access to treatment and medication is delayed – often days, sometimes weeks – resulting in confusion, Rx Abandonment, and an overall dissatisfied experience with the doctor.
A Technology Gap
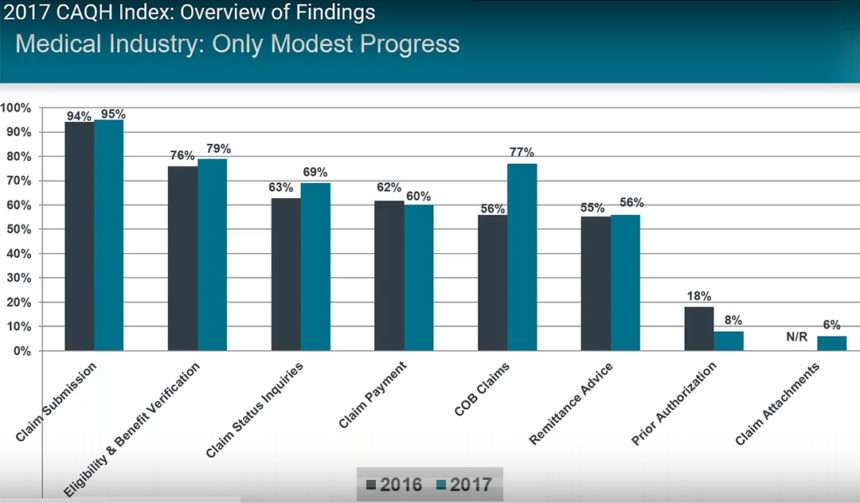
This CAQH graph shows industry wide adoption rates of each electronic HIPAA transaction type
Although 87% of primary care physicians have adopted EHR, and 70% e-prescribing, and although adoption of electronic claim submission is at 95%, the adoption rate for transmitting prior authorization digitally is just a shocking 8%, meaning that as of today, 92% of pre-authorizations are being done manually via phone and fax.
If PA is so hated and the bane of every practice’s existence, where lies the disconnect?
The Ugly Truth
A significant technology gap exist due to the inability of software makers to reconcile the incomprehensible variables of over 2000 health plans that each have their own prior authorization request form. But the standardized form for electronic precertification, the ANSI 278 Services Authorization, has been in place since 1996 by HIPAA regulations, and is now overseen by the NCPDP ePA data exchange standard.
But unlike electronic claims, e-prescribing and eligibility, States have not forced insurance payers to adhere to long established standards, so doctors were simply left to bear the cost burden of an industry-wide problem of no form standardization enforcement––to the tune of $23 billion dollars a year. When you look at an insurance company skyscraper (that incidentally takes up an entire city block of the financial district), and compare it to a family doctor’s small office, this is a difficult pill to swallow. Rather than a technology gap, what we seem to have is an integrity gap on the part of the insurance industry.
But Doctors Have Done Their Part
21 Principles To Better Care: In Jan 2017, in an attempt to take on PA rules that hinder patient care, the AMA and a coalition of 16 other healthcare associations representing physicians, medical groups, hospitals, pharmacists, and patients drafted a comprehensive plan to simplify the PA process by offering 21 principles to reform PA requirements. These patient centered principles are divided into five categories:
- Clinical validity – Is UM criteria based on up-to-date clinical criteria
- Continuity of Care– Current medical treatment or prescription drug regimen should not be interrupted while the utilization management requirements are determined
- Transparency and Fairness – Medical necessity review entities should provide accurate, patient-specific, and up-to-date formularies, along with detailed explanations for denials, especially on non-formulary drugs
- Timely Access – Establish maximum-response times for UM decisions so that patient care is not disrupted
- Alternatives and exemptions – As Principle # 21 states: “A health care provider that contracts with a health plan to participate in a financial risk-sharing payment plan should be exempt from precertification and step-therapy requirements for services covered under the plan’s benefits.”
The 21 principles attempt to make PA patient centered rather than focused purely on profit.
So, in the light of industry wide failed ePA adoption, how does one explain the success of electronic claims, and electronic prescriptions?
Adoption of electronic claims is explainable as over the last twenty years, one by one States required insurances to adopt the CMS-1500 claim form as the standard for all insurance claim submission – both public and private – and then they legislated that all claims be submitted electronically – except by exception request.
Wide adoption of electronic prescription ordering is explained by the fact that in 2001 pharmacy associations formed Surescripts to create a link to physicians, and replace paper prescriptions with more accurate e-prescribing. Then in 2009, The HITECH ACT activated doctors to adopt EHR which also contained ePrescribing modules.
Electronic prescriptions avert millions of medication errors each year (17.4 million errors last year alone), and today, States are averting a controlled substance crisis by reining in prescription fraud through implementing of the e-prescription system, thus showing the efficacy of electronic solutions.
The Advent of Electronic Authorizations
Only recently have a handful of payers and software vendors bridged the gap of electronic PA.
Although individual payer rules still exist in the hundreds of thousands, and prior review form differences amount to the thousands, recently 70 of the largest payers (such Blue Cross Blue Shield, United Health Care, AETNA, CIGNA, and HUMANA) have adopted the ANSI 278ePA standard, which has been in use by the The Centers for Medicare & Medicaid (CMS) for years now.
Even though ANSI 278 standards for ePA, along with similar HL7 Protocols have existed for a while, the recent move by the larger healthcare payers makes it possible for software vendors to organize the PA form process, and include ePA as part of integrated clinical EHR records. But as demonstrated above, adoption is painfully slow as the electronic approvals are only now seeing the light of day.
A New Process
But, ePA can now be automated to the point where the software program can recognize a CPT code or hcpcs code, match it up with payer rules to determine necessity, and then submit required data gathered from the encounter notes and transmit for prior approval: For diagnostic orders, DNA testing, medication, procedures and devices; without the effort of the clinical or office staff.
A New Process
But, ePA can now be automated to the point where the software program can recognize a CPT code or hcpcs code, match it up with payer rules to determine necessity, and then submit required data gathered from the encounter notes and transmit for prior approval: For diagnostic orders, DNA testing, medication, procedures and devices; without the effort of the clinical or office staff.
And in the best ePA systems, a physician can now: Order diagnostics, diagnose a problem, prescribe, and (in a perfect world) recommend a treatment plan – all without ever have to interact with the insurance carrier because now software is managing the entire prior consent process in an automated fashion, beginning-to-end.
Prior Authorization Software Checklist
An ePA system must be able to:
- Process both Rx authorizations (ANSI 272), and medical service authorizations (ANSI 278).
- Be Stage 3 Meaningful Use compliant regarding interoperability.
- Access the patient’s insurance status and reach out to the payer to determine if PA is required.
- Initiate the approval process if determined a requirement.
- Alert the clinician and/or staff that it has initiated the process with an at-a-glance dashboard status.
- Autofill the patient’s information and the physician’s information.
- Prompt the physician to add any additional information necessary for a successful request.
- Track status of all in-progress authorizations.
- Prompt an administrator when authorizations are delayed or stalled.
- Provide a dashboard that clearly displays the status of all current, past, and denied authorizations.
- Send alerts when an authorization needs attention from an administrator.
- Allow the user to easily capture local payer rules and either contribute them to the main database or use them locally.
- Allow users to exchange data with payers using either APIs or EDI 278 transactions.
- Customize the system to fit the practice’s workflow.
The reality is that a true beginning-to-end authorization solution involves a tight integration with a practice’s EHR and billing software—no small order. It is being done, but the current state of technology means that for many practices, a hybrid outsourcing model is preferred, where a software application is used in the office to request and monitor PA status, while back end services are rendered by a team of PA experts that ensures each authorization is pushed through and obtained.
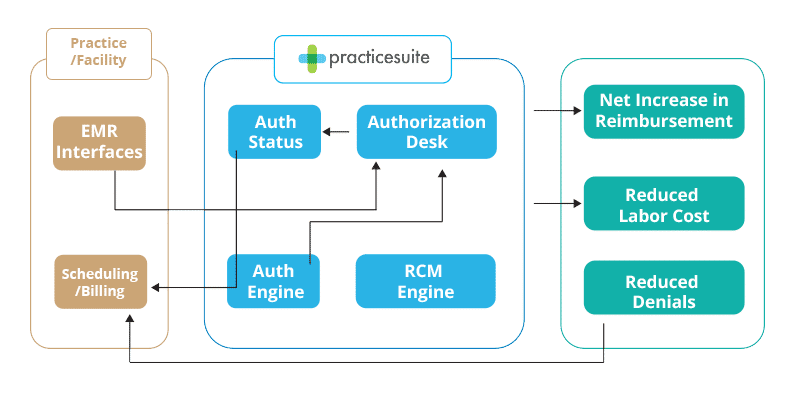
Closed Loop Authorization Process Flow
Outsourcing Prior Authorization
Prior approval is a headache for providers and patients alike. But interestingly, one thing physicians and payers agree on is the need to adopt ePA to streamline the system. Here we take a look at the pros and cons of employing third-party software and services to reduce cost and speed up the authorization process.
Advantages & Disadvantages
Advantages : A 2017 survey published by CoverMyMeds found that providers who used only an electronic method for PA requests spent 2.5 fewer hours on authorizations on average each week but that only 24% respondents rely solely on ePA.
Disadvantages : Unfortunately, while technology can potentially speed up the PA process, it’s not easy for providers to find and implement an authorization system that truly fully manages the process—and that works with their existing practice management system and EHR. And although an astounding 96% of payers said they are committed to fully electronic automated solutions to help solve their determination process, change is slow.
When is outsourcing right for your practice?
If you or someone in your practice takes the time to add up all the hours spent requesting prior approvals and compares that cost to the cost of paying a third party, you’ll have a clear-cut answer to the question of outsourcing. Additionally, the time freed up can amount to hours per week to see more patients.
4 Reasons Its Time To Outsource PA
- If costs are in fact reduced,
- If nurses and administrative staff are freed up to focus on serving patients,
- If patients receive more timely care as a result of faster authorization turnaround,
- If the result is recovered time to see more patients, there’s little question as to the value of outsourcing.
What are the main benefits of outsourcing?
In addition to improving the patient experience by having authorizations go through quickly and freeing up staff for more important (and less frustrating) tasks, prior authorization specialists can help reduce the number of rejected and denied claims, which can increase reimbursements and reduce days in A/R.
Full service companies also make it their business to track all changes in Medicare, Medicaid, and third-party payers, greatly improving your billing compliance levels.
Do certain specialties stand to gain more from outsourcing?
Internal medicine practices certainly have the potential to benefit from outsourcing PA. However, specialty practices and standalone specialty clinics may be the organizations with the most to gain from outsourcing.
For example, oncologists frequently order test that require authorization—such as complex MRIs, ultrasounds, and CT scans—to help them determine the best therapy for their patients.
Similarly:
* Cardiologists frequently run into denials when they prescribe PCSK9 inhibitors, direct oral anticoagulants, and angiotensin receptor-neprilysin inhibitors.
* Allergists and dermatologists find it difficult to get approval for the biologics they prescribe when traditional therapies fail those with psoriasis, asthma, atopic dermatitis, and urticaria.
* Psychiatrists face multiple problems related to prior review, including medication renewals and emergency admissions to psych units.
* Oncologists and other specialists ordering genetic and molecular tests for patients are having so much trouble getting authorization that some labs are performing the tests prior to receiving approval—on the basis of supporting good patient care and knowing they may not be paid.
Important questions to ask prospective vendors
The most important question to ask is what type of authorization services the vendor provides. Some vendors provide only prescription authorizations ANSI 272, which is fine if you plan only to outsource Rx and keep service authorizations in-house. But if you frequently need to obtain PA for labs and diagnostics, treatments, and/or medical equipment – all ANSI form 278 – you’ll want a vendor that provides a full range of PA services.
Of course, you’ll want to determine exactly what software features will be provided and services the vendor will perform and the costs for those services. Beyond that, here are some details you may want to explore:
- Does my practice need to have any involvement in the initial PA process?
- Will I or my staff be alerted when a PA is automatically initiated, and can we specify to whom those alerts go?
- How will we be notified when additional information is required for authorization, and how is that process handled?
- How can my staff keep track of the PA submissions we have in progress?
- How does your company handle local payers you may not have worked with before?
Finally, you’ll want to ask about the reports your software / service vendor will supply to show how many authorizations get approved on the first try and how quickly denied approvals are appealed and approved.
[Sources: “2017 AMA Physician Survey,” American Medical Association, //www.ama-assn.org/sites/default/files/media-browser/public/arc/prior-auth-2017.pdf “2018 ePA National Adoption Scorecard, CoverMyMeds, //www.covermymeds.com/main/insights/scorecard/ ]
Who are the vendors offering PA applications?
Prior Authorization Reviews
Despite clamor from providers regarding the convoluted, highly manual pre authorization process, electronic PA solutions are still only sparsely used and mostly by larger organizations.
Features included in these solutions vary, as do costs. But to help you sort through the options, following is our review of the top seven vendors offering ePA solutions.
#1. First on our list is PracticeSuite a cloud-based Stage 3 Meaningful Use Certified EHR and Practice Management platform for ambulatory care that offers unlimited plug and play applications and interoperability. Its pre authorization product AUTHORIZATION DESK can be used as a stand-alone application or in conjunction with any Stage 3 EHR or compliant medical billing system. The application determines necessity, submits authorization, monitors status, organizes requests into queues (open, pending, completed), and notifies staff and clinicians of next steps. Platform supports multi-location, multi-specialty, and the ability to restrict access by role, patient, user, time and location. PracticeSuite’s expert services team delivers 94% of authorizations with no action required by the client. (Read our full review).
#2. Availity Authorizations covers all three steps of the authorization process, and checks CPT-specific request against a robust knowledgebase of payer requirements. It then submits the authorization (unless additional clinical input is required), and pings the payer behind the scenes until it receives notification. (Read our full review)
#3. AzaleaHealth is a cloud-based Health IT platform that offers Pre-authorization Services for obtaining PA for inpatient and outpatient procedures in addition to pre-certifications for hospital admissions. Their experienced customer service staff transmit patient data back to the appropriate areas within the healthcare organization. A web-based portal allows for transparency and single-screen management, status-based filtering, procedure code look-up and email notifications of completions and status updates. (Read our full review)
#4. CareConnections specializes in physical therapy clinical software and as part of their therapy suite provides a web-based PA systemPAS, that offers the ability to review or authorize therapy services, and it simplifies referral coordination. Their “Clinical Practice Guidelines: Examination & Intervention for Rehabilitation – 4th Edition” is offered free in conjunction with their PAS services. (Read our full review).
#5. HEI Global Health : As the name suggests, HEI is a global service and software organization with expertise in both Revenue Cycle Management and Clinical Information Systems, offering Cerner integration for PA. (Read our full review).
INFINX serves hospitals, imagining centers, laboratories and clinics, using AI & HI (human intelligence) to manage an organization’s entire payment lifecycle. Software includes a laboratory information system (LIS) combined with revenue cycle management services, including PA for molecular and genetic testing laboratories, as well as solutions for radiology.
PriorAuthNow is a cloud technology that helps providers obtain fast determinations; payers automate authorization determinations; laboratories automate complex authorization requirements; and manufactures increase patient access to specialty drugs, medical devices and equipment. Its solution helps reduce wait times for authorizations, with some coming back in real time. All PA requests are submitted and monitored electronically from a single dashboard location.
Rx, Web-Portal Solutions
Agadia PAHub a HITRUST certified Rx solution automates the end-to-end management of prescription authorizations across healthcare services, channels, and lines of business. It features real-time integration with leading enterprise systems, EMR vendors, and physician portals.
CenterX This Rx solution notifies prescribers when PA is required through proactive alerts during order entry. It pulls data directly from the provider’s EHR into standardized authorization forms, reducing dual documentation, and it integrates with the provider’s patient portal, allowing clinicians to automatically notify patients when their medication is approved and ready for pick up.
CoverMyMeds electronically connects providers, pharmacists, and plan/PBMs. This Rx solution improves time to therapy and decreases prescription abandonment. Providers can initiate PA requests using an onlineportalor at the point of prescribing through one of the EHR vendors integrated with the solution.
IIC is a cloud-based payer technology that allows insurance companies to immediately approve PA submissions. They also offer healthcare providers a web-portal to check patient eligibility and benefits (EDI 270), and send referrals and authorization via EDI 278 to obtain payer approval for medical procedures, tests, labs, equipment (DME), pharmaceuticals, hospital admissions and extensions, and expensive drugs covered under medical benefits; as well as outpatient procedures, inpatient admits, stay extensions, DME, tests, labs, drugs, that are either approved or denied based on the payer policy guidelines (medical necessity and/or appropriate use criteria).
MCG Cite AutoAuth is a clinical information company that provides evidence based clinical decision support for health payers via a web-based interface that also allows providers to receive an expedited response via an insurance’s web-portal. The system also makes it easy for providers to document and support treatment requests.
SureScripts, the nation’s Rx backbone, offers a PA product formally called CompletEPA. that integrates directly with electronic health records (EHRs), and enables healthcare professionals to easily obtain Rx authorizations in real time at the point of care, thereby eliminating paper forms, faxes, and phone calls. Their online portal provides a free way to easily submit fully electronic PA requests even if service is not yet available within your EHR.
Prior Authorization Calculator
Calculate the Impact Prior-Auth is Having on Your Practice

Recent Legislation on Form Standardization
The government, mainly in the form of CMS, has been for years pushing hard on healthcare entities to improve care while lowering costs. Recently, experts pointed at preauthorization as an excellent new target.
On July 31, the Senate health committee held a hearing on administrative costs where Harvard economics professor David Cutler estimated that streamlining billing systems could cut the health system’s administrative costs in half. He recommended standardizing prior notification forms for all insurers, eliminating extraneous billing codes, and directing the integration of EHRs and billing systems so that patients’ health histories are automatically linked to treatment authorization.
Cutler told the senators that since government is the biggest payer, it needs to be the one to standardize and simplify coding. He also likened administrative costs to an “arms race,” saying that when insurers are pushed to reduce spending, they introduce requirements providers must fulfill to get paid. In response, providers hire personnel to maximize reimbursement and, seeing this, insurers beef up the rules again.
According to Modern Healthcare, several senators agreed that obtaining authorizations are a major issue for providers. Senators Hassan (D-NH), Murkowski (R-Alaska), and Cassidy (R-La.) criticized the health insurance industry for the way it currently treats treatment authorization and said insurer’s verification requirements can place undue burden on patients and physicians while threatening delays in medical care.
The Senate committee plans to consider creating legislation that would regulate how health insurers handle prior authorizations. Senator Smith (D-Minn.) said she’s working legislation to support public-private partnerships as a way to demonstrate success in standardization efforts.
One such effort is a collaboration of more than 130 health plans, hospitals, and vendors that was recently endorsed by the Council for Affordable Quality Healthcare (CAQH) and the Committee on Operating Rules for Information Exchange (CORE), a not-for-profit that aims to help stakeholders adopt standardized electronic transactions.
“Substantially improving prior approval on behalf of the industry ranks among our highest priorities in 2018,” says CAQH CORE, adding that because requirements to obtain precertification for miscellaneous items has a significant impact on healthcare costs and continuity of care, it has been working extensively to address the issue through CAQH CORE Operating Rules and Certification.
Industry efforts notwithstanding, the panel will no doubt consider Cutler’s strong emphasis on the role of government. He says that while payment reform and IT promotion (both part of the HITECH Act) are important areas, they would be more effective if seen as part of a larger goal: creating and implementing a plan to reduce the administrative costs of medical care.
“The reality of the situation is this,” he says, “Unless the federal government leads the way, the United States will continue wasting hundreds of billions of dollars annually on unnecessary administrative expenses. I urge Congress to act to prevent this.”
Stepping Away from Step Therapy
Step Therapy Denials
Insurers call it step therapy; critics call it fail first—and the contrast between those terms makes healthcare’s deep divide on this topic abundantly clear. The problem is that, on paper, step therapy seems perfectly reasonable. The patient must try a generic version of a drug or less expensive therapy before being approved for a more expensive drug or therapy. The reality is something completely different.
In the past few years, physicians have encountered situations where step therapy has caused patients serious injury and, in some cases, increased their risk of dying. Dr. Kenneth Blankstein, a New Jersey oncologist, told Stat News about a lung cancer patient. Because she responded well to the first chemotherapy drugs he prescribed, he gave her a temporary break when her health stabilized. When he tried to return her to treatment, the insurer said the break was evidence the treatment had failed and demanded she move to a different treatment.
“The patient’s being told to use a drug we know isn’t going to work, but we have to use it anyway for someone with terminal illness? To me that’s just insane, but it’s the way they do things,” Blankstein said. “It’s taken away clinical judgment. It’s managing by algorithms.”
Reducing frustration through transparency
Healthcare experts agree that step therapy has been on the rise in the last decade. A Milliman report sponsored by Pfizer found that total formulary restrictions increased from 41% in 2011 to 76% in 2016. One reason for the increased restrictions and mounting physician frustration is increased use of high-priced biologic medications.
Physicians argue that restricting biologic use is penny-wise and pound foolish. Initial costs may be high, but overall costs are lower if patients stay healthier and avoid additional treatments and/or hospitalizations.
There are no federal laws that address step therapy, and state laws vary widely. Indiana’s law is the strictest, according to the National Patient Advocate Foundation, barring insurers from restarting the step-therapy sequence if a patient has failed certain treatments with a previous insurers. In addition, insurers must adjudicate appeals within three days.
That fast turnaround, along with increased transparency, is the key to solving the step-therapy issue, say many physicians. Today, reform efforts at the state and federal level are centered around:
- Requiring health plans to provide a reason other than cost for denying coverage of a prescription drug
- Giving physicians the option to override the health plan’s decisions if the treatment option identified by the insurer is likely to be ineffective based on the patient’s medical history or clinical practice guidelines.
- Requiring more advanced, standardized communication around the step- therapy process so that adjustments and exceptions can occur quickly.
In addition to advocating for federal and state laws aimed at step therapy reform, clinicians interviewed by PM360 recommended the following to improve the chances that patients will receive the best treatment without delay
- Use generic and/or formulary medications where appropriate (the idea is to strengthen the credibility of the prescriber when he/she orders a non-generic or non-formulary drug––a medication that’s not on the authorization list for member benefits).
- Thoroughly document your rational for prescribing a specific agent using clinical practice guidelines and (where possible) randomized clinical trial data.
- Document the authorization request process in detail for each patient. In some cases, practices can receive special status that exempts them from routine PA by demonstrating a low rate of denials.
Dr. Steven Pearson, founder of the Institute for Clinical and Economic Review put it this way: Most people would say it’s reasonable to try the less expensive or non formulary drug first in a situation where two treatments would likely offer equal benefits. “The important nuance comes when there might be specific reasons where a patient or doctor feels like the more expensive drug would work better. So it all depends on what the harm would be if they tried the less expensive one first.”
Preauthorization for Dummies
But just how many different types of PA are there?
The short answer is too many, but the grand division lies between prescriptions, and medical services covered under a health benefit plan, referred to as medical authorizations. Doctors must obtain PA for surgical procedures, durable medical equipment, expensive or controlled prescriptions, physical therapy, referral to a specialist, radiology and diagnostic testing, and something new, molecular and advanced diagnostic genetic testing.
Simplified; the permission-approval process is three and a half steps:
- Determination – Does this particular payer require a PA for this procedure, medication, or device. ePA software accomplishes this almost instantly by looking at tables of data supplied by the insurance carrier.
- Requesting Approval, PA Form Submission – software has been handling form-submission for decades. Now that a standardized form is in play – problem solved.
- Status Monitoring and Appeals – While the payer determines whether this is the right test or treatment for the right condition on the right patient, the software is on the lookout for status updates from the payer. Once received, it then updates the secure web portal solution and initiates the next step as required. Approved, you have your PA. Denied, you correct and resubmit.
Prior Authorization Denied –Top Three Reasons
Of the top ten reasons for denied authorizations, all are due to absent minded errors such as missing or incorrect patient demographics. You can greatly speed up the PA process by taking the following steps:
- Make certain all relevant fields are completed (accurately)
- Make certain F/L Name, DOB, Sex, and SSN are present and correct
- Make sure the CPT code for which approval is sought agrees with age and sex
Denials In Radiology & Imaging
No PA means a denial is inevitable. And a medical specialty hit especially hard by PA denials is Radiology and Diagnostic Testing where a physician needs evidential data in order to form a diagnosis. The area is controversial because the doctor is reasoning from training and experience whereas the payer is operating from actuaries – or in other words care vs profit. Again here the hospital or provider are assured of a denial unless a PA is obtained, but in this setting, time is of the essence. Only ePA can address this time sensitive problem as approval can be obtained electronically in minutes or hours.
In a precertified procedure, when the covered entity has received permission from a third party authorization (TPA) for the correct CPT, the tpas then forwards the coordination of benefits and acknowledges the precertification completion for the approved authorization request form.
Technology Developments
Other technology developments today are interactive prior-approval criteria which allow real-time pharmacy benefit transactions (RTPB) and the capability to obtain approvals in minutes and hours, not days. And applying robotic processing automation (RPA) to repetitive, transactional and rule-based processes to help streamline operations, reduce the time to complete tasks, improve the customer experience, and lower labor costs.
ePA Software
What can electronic (ePA) or automated precertification software do? A look at the complex world of Labs and RAD shows how software provides a solution. While the industry tends to focus on prescriptions, authorizations for treatment can be more complex, time consuming, and impact treatment equally if not more. This in-depth analysis looks at the problem areas of Testing and Radiology, which have complex PA notification needs; and may also require PA services in addition to software automation; such as in the case where an insurance does not have the capability to receive electronic PA, but coverage determination is needed within business days rather than calendar days, and quantity limits are set in place for the non-breaching party.
Learn more about current PA legislation.





