The Practice of the Future, Today
Patient needs have evolved. Let's catch you up.
Practice Management Software
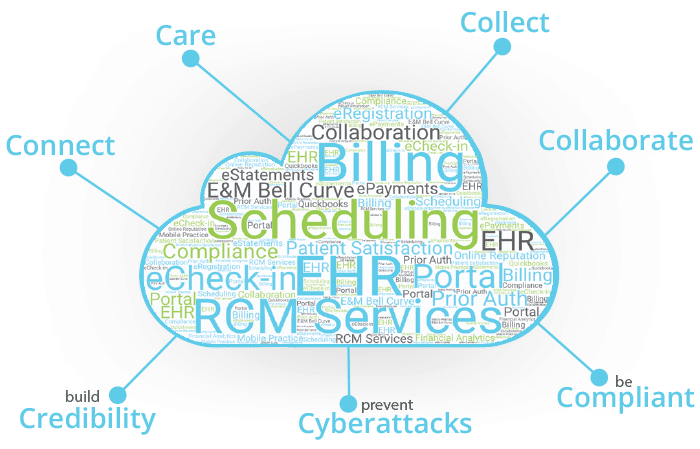
Adopt a single cloud based office solution to care, collect, connect, collaborate, build credibility, prevent cyberattacks, and be compliant.

Offer Patients a Modern Digital Communications Experience
Better Patient Communication
begins by engaging patients the way they need and prefer. Save time and money while practicing more efficiently with Secure Text, eRegistration, Telehealth, Automated Reminders, Mobile Check-in and ePayments.
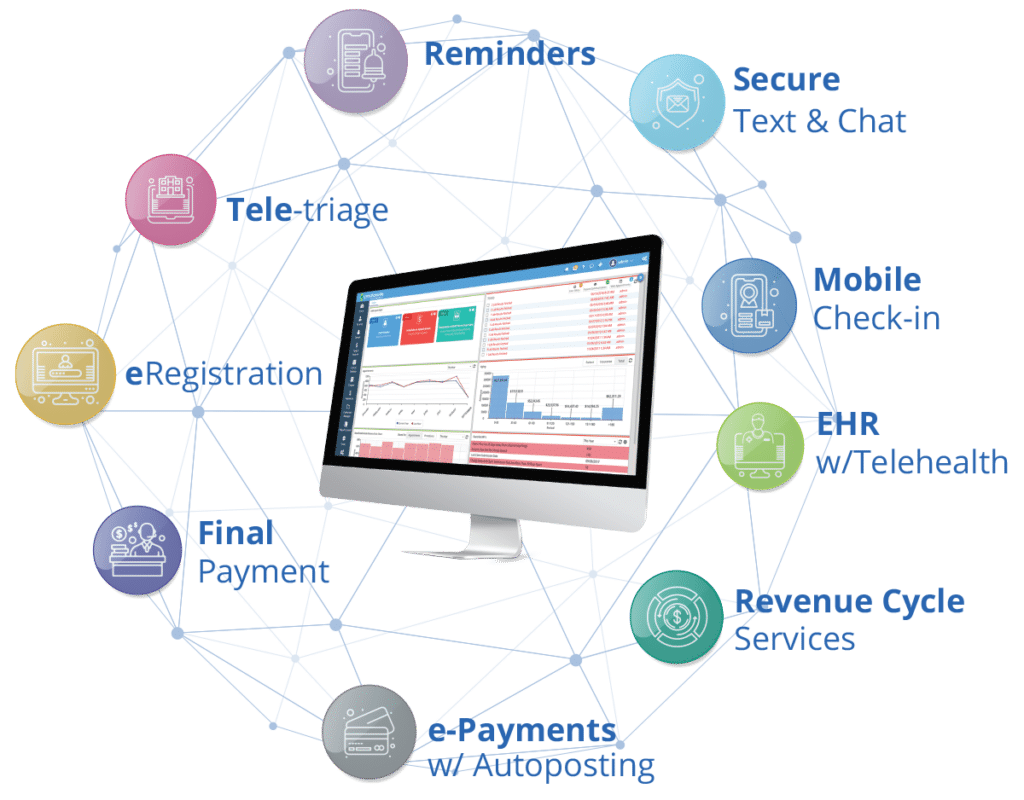
Manage Your Entire Practice On a Single Enterprise Platform
Multi-location Scheduling & Practice Management
EHR w/ Telehealth +61 Specialties
Gold Standard RCM Services
Patient Communications, Group Messaging
Electronic Registration & Check-in
Medical Billing Software Engineered for RCM
e-Statements with a Quick-Pay link
Robust Financial Reporting, KPI's by Role & Dept.
Manage Your Entire Practice On A Single Platform
With an affordable all in one solution for in-office and remote patient care. PracticeSuite provides flexible workflows to help organize your practice and keep it operating at peek efficiency; as well as a complete end to end virtual practice that allows you to treat any patient, anywhere, on any device.
Multi-location Scheduling & Practice Management
EHR w/ Telehealth +61 Specialties
Gold Standard RCM Services
Patient Communications, Group Messaging
Electronic Registration & Check-in
Medical Billing Software Designed Specifically for RCM
e-Statements with Quick-Pay Link
Robust Financial Reporting, KPI's by Role & Dept.
Partnering Into The Future
RCM Billing Services
Improve reimbursements with PracticeSuite's expert medical billing services team. Schedule a 1:1 meeting.
Learn MoreEHR w/ Telehealth
Certified EHR with Remote Patient Care. Secure Video & Phone Consult within Chart. Concierge Support. Full Service Back-office Billing.
Certified EHRA Central Billing Office for groups and multi-location practices
Improve your time-to-payment and overall revenue collections with medical billing software designed specifically for revenue cycle management.
Learn MoreCloud Based Practice Management Software
Manage your entire medical practice, decrease no-shows, and improve cash collections.
Learn MoreElectronic Payment Services
Speed up patient payments with convenient in-person, online payments, and options like card-on-file and payment plans.
Learn MoreeRgistration & Mobile Check-in
Offer a modern digital patient experience with online Registration, office messaging, and Mobile Check-in.
Learn MorePatient Engagement
Stay connected with your patients by improving communications. Give them access to their records and other online services.
Learn More
Partnering For The Future
WHO WE ARE
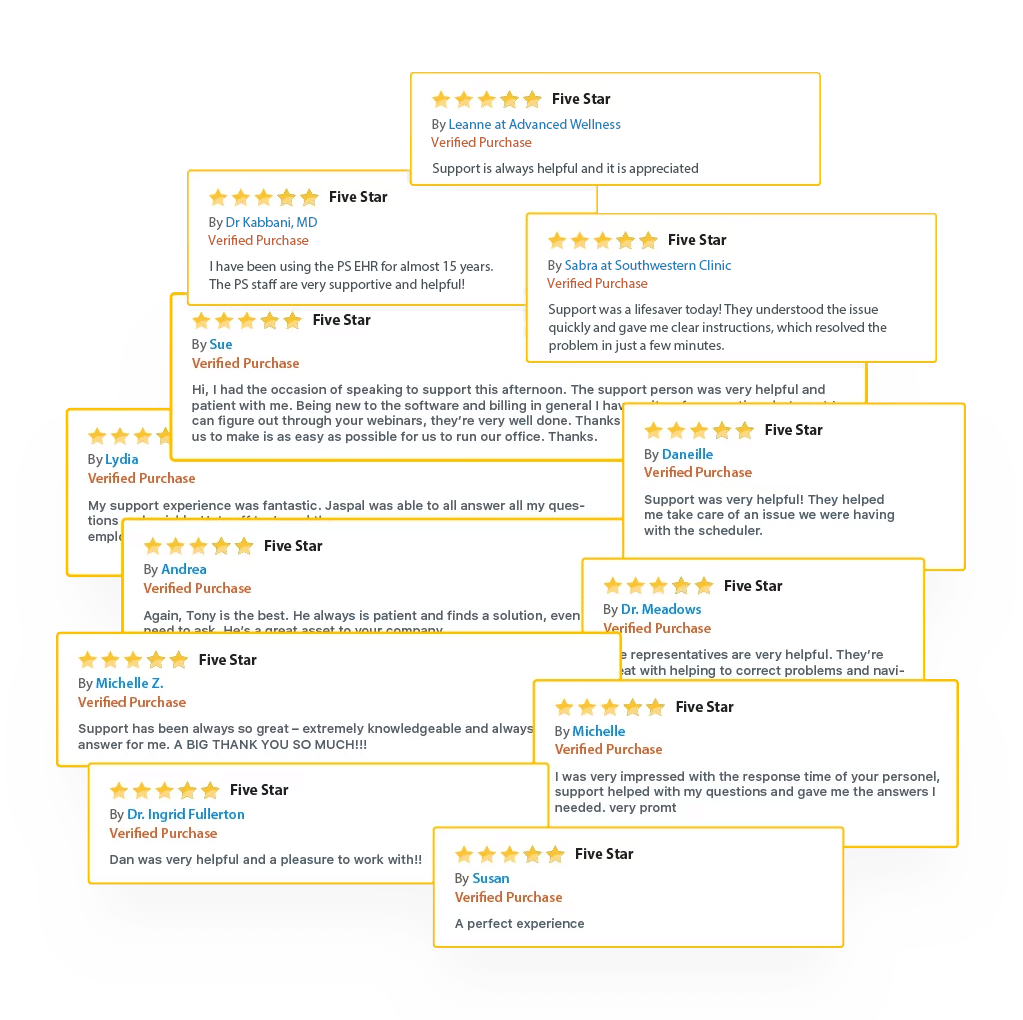
We’re not surprised. For the last 15 years we’ve grown primarily by client-recommendation rather than incurring millions in advertising costs. Instead, we’ve dedicated our resources to what matters most: Great practice management software, fantastic support and a team of over 200 people dedicated to keeping your practice up and running day in and day out.
WHO WE ARE
We’re not surprised. For the last 15 years we’ve grown primarily by client-recommendation rather than incurring millions in advertising costs. Instead, we’ve dedicated our resources to what matters most: Great practice management software, fantastic support and a team of over 200 people dedicated to keeping your practice up and running day in and day out.
What Are Others Saying About Their Experience ?

Learn from medical practices, physicians, and medical billing services about the value of PracticeSuite’s people and products.


When difficulties arose,
how did we do?
The Human Touch Behind The Hi-Tech
The Human Touch Behind The Hi-Tech
Security, Resilience and
High Availability
- A single-source, all in one office solution
- Unparalleled SOC2® security
- Flexible: For solo practices to large groups
- Enterprise technology. Designed to always run
Safeguard and futureproof your practice with a single-vendor practice management solution that reduces software cost, increases practice revenue, improves staff efficiency, and enables anywhere access to patient care.

Our Certifications,
Compliance & Governance
PracticeSuite is a complete practice management solution featuring medical billing software designed for enterprise revenue cycle management, that has achieved SOC2® Data Security Certification, and offers an ONC Certified Stage 3 EHR with Cures Update, and provides large groups and multi-location practices with a central billing office with integrated electronic payments and patient engagement tools that create a modern digital patient communication experience for your practice.









Built on a Foundation of Enduring Technologies








The Smart Medical Practice
Transitioning From Quest Quanum to PracticeSuite Helps Physicians Avoid Major Disruption
TAMPA, Fl., Oct. 03, 2023 – Quest’s Quanum EHR is being sunsetted at the end of this year. For many physicians, that date is too close for comfort. Quest made
PracticeSuite Provides Painless Migration to Its Cures Ready EHR for Quest Quanum Clients
TAMPA, Fla., Feb. 2, 2023 [NEWSWIRE] On 1/24/23 Quest Diagnostics began notifying its EHR clients that they are sunsetting their QuanumEHR by the end of 2023. Meanwhile PracticeSuite has stepped
PracticeSuite Achieves ONC 21st Century Cures Certification
PracticeSuite, Inc., a leading cloud platform for ambulatory care providers, announces the Office of the National Coordinator of Health Information Technology (ONC-HIT) certified PracticeSuite ambulatory electronic health record (EHR) for
PracticeSuite Is SOC2® Certified
PracticeSuite, Inc., an end-to-end medical office solution for ambulatory medicine, attains SOC2® TYPE 1 Security Certification—the coveted gold standard in data security, demonstrating its dedication to excellence in process monitoring, encryption
5 Must-Have Medical Practice Management Software Features for Better Workflow Productivity
Efficiently running a medical practice, whether a physician’s office or a larger multi-specialty clinic, requires the implementation of essential administrative routines. While doctors play a crucial role in patient’s lives,
Key Features of Medical Practice Management Software
As medical practices become more complex and patients demand better care, medical professionals are turning to practice management software to help streamline workflows, improve productivity, and reduce errors. According to Data

